Abnormal results from Pulmonary Function Tests (PFTs)
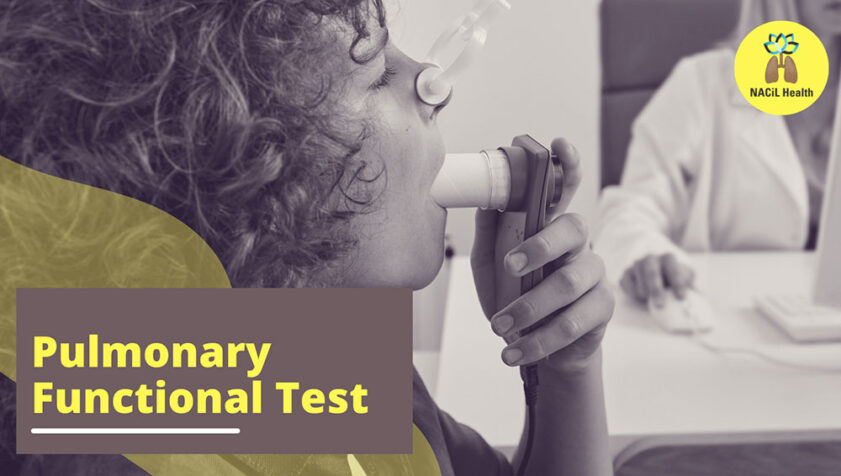
Pulmonary Function Tests (PFTs) are a set of non-invasive tests that assess how well your lungs are working. These tests measure lung volume, capacity, rates of flow, and gas exchange. The results can help your healthcare provider diagnose and decide the treatment of certain lung disorders.
Common Components of PFTs:
- Spirometry:
- What it measures: The amount (volume) and/or speed (flow) of air that can be inhaled and exhaled.
- Procedure: You’ll be asked to breathe in deeply and then exhale forcefully into a mouthpiece. This test can measure the forced vital capacity (FVC) and forced expiratory volume in one second (FEV1), which are crucial for diagnosing conditions like asthma, COPD, and other restrictive or obstructive lung diseases.
- Lung Volume Measurement:
- What it measures: The total volume of the lungs and how much air remains in the lungs after exhaling fully (residual volume).
- Procedure: This might involve breathing in and out of a closed system while pressure changes are measured or using techniques like body plethysmography.
- Diffusion Capacity (DLCO):
- What it measures: How well oxygen moves from the lungs into the blood.
- Procedure: You’ll breathe in a small amount of a tracer gas (like carbon monoxide), hold your breath for a brief period, and then exhale. The amount of gas exhaled is measured to see how much was absorbed by the blood.
- Bronchodilator Tests:
- What it measures: The reversibility of airway obstruction.
- Procedure: After performing a spirometry test, you might be given a bronchodilator (a medication that opens up the airways) and then retested to see if your lung function improves.
- Oxygen Level Tests (Oximetry):
- What it measures: The level of oxygen in the blood.
- Procedure: A small device (pulse oximeter) is placed on your finger or earlobe to measure oxygen saturation.
When PFTs Are Used:
- Diagnosis: To diagnose conditions like asthma, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, and other respiratory disorders.
- Monitoring: To track the progression of lung diseases or monitor the effectiveness of treatment.
- Pre-surgery Assessment: To evaluate lung function before major surgery.
Preparing for a PFT:
- Avoid heavy meals before the test.
- Refrain from smoking or using bronchodilators as advised by your healthcare provider.
- Wear loose-fitting clothing that doesn’t restrict your breathing.
Interpreting PFT Results:
- Normal Results: Indicate that your lung function is within the expected range.
- Abnormal Results: Could suggest a respiratory condition, but your healthcare provider will consider your medical history, symptoms, and other tests before making a diagnosis.
Abnormal results from Pulmonary Function Tests (PFTs) can indicate various types of lung disorders. These results are typically classified into three main categories: obstructive lung disease, restrictive lung disease, and diffusion abnormalities. Here’s what each might indicate:
- Obstructive Lung Disease:
- Description: This type of abnormality is characterized by difficulty in exhaling all the air from the lungs due to narrowed airways.
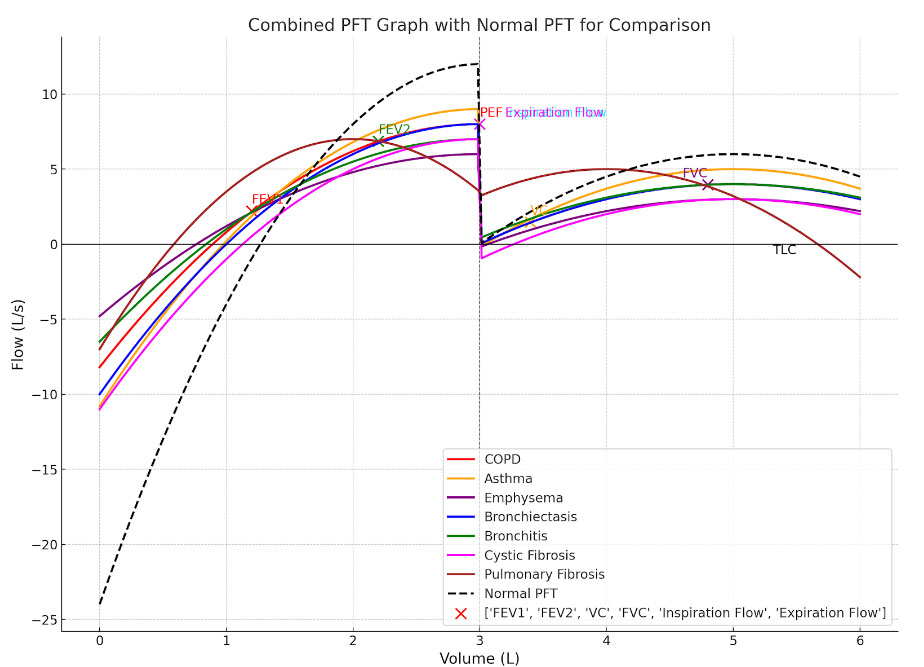
- Common Conditions: Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchitis, emphysema, and bronchiectasis.
- Key PFT Findings:
- Reduced FEV1 (Forced Expiratory Volume in 1 second): This measures how much air you can forcefully exhale in one second. A lower-than-normal FEV1 suggests obstructive disease.
- Reduced FEV1/FVC Ratio: The ratio of FEV1 to Forced Vital Capacity (FVC, the total volume of air exhaled) is reduced. A ratio less than 0.7 (or 70%) is commonly indicative of obstruction.
- Normal or increased TLC (Total Lung Capacity): Despite obstruction, the lungs might remain hyperinflated, leading to an increased TLC.
- Restrictive Lung Disease:
- Description: Restrictive lung disease is characterized by a reduced ability to fully expand the lungs, leading to decreased lung volumes.
- Common Conditions: Pulmonary fibrosis, sarcoidosis, interstitial lung disease, obesity-related lung issues, and neuromuscular diseases affecting lung expansion.
- Key PFT Findings:
- Reduced FVC (Forced Vital Capacity): This measures the total amount of air exhaled after a deep breath. In restrictive lung disease, the FVC is lower than normal.
- Normal or increased FEV1/FVC Ratio: Because both FEV1 and FVC are reduced proportionally, the ratio may be normal or even slightly increased.
- Reduced TLC (Total Lung Capacity): A significantly lower TLC is a hallmark of restrictive lung disease.
- Diffusion Abnormalities:
- Description: These abnormalities involve issues with gas exchange in the lungs, particularly the movement of oxygen from the alveoli into the bloodstream.
- Common Conditions: Emphysema, pulmonary fibrosis, pulmonary hypertension, and conditions that affect the alveolar-capillary membrane.
- Key PFT Findings:
- Reduced DLCO (Diffusing Capacity of the Lungs for Carbon Monoxide): A low DLCO indicates problems with gas exchange, which can be caused by damage to the alveoli, thickened alveolar walls, or decreased blood flow in the lungs.
Interpretation of Abnormal Results:
- Low FEV1 and FEV1/FVC Ratio (<70%):
- Suggests obstructive lung disease. The severity is often graded based on how much the FEV1 is reduced:
- Mild: FEV1 ≥ 80% predicted
- Moderate: FEV1 50-79% predicted
- Severe: FEV1 30-49% predicted
- Very Severe: FEV1 < 30% predicted
- Suggests obstructive lung disease. The severity is often graded based on how much the FEV1 is reduced:
- Low FVC with Normal or High FEV1/FVC Ratio:
- Suggests restrictive lung disease. Further tests like measuring TLC and lung volumes are needed to confirm the restriction.
- Low DLCO:
- Indicates a problem with gas exchange, which may be due to conditions affecting the alveoli or pulmonary blood vessels.
Combined Patterns:
- Mixed Obstructive and Restrictive Pattern: Some individuals may exhibit both obstructive and restrictive patterns, such as in cases of combined COPD and pulmonary fibrosis.
- Reduced FEV1, FVC, and TLC with Low DLCO: This could suggest a severe, advanced lung disease, possibly involving both the airways and the lung parenchyma.
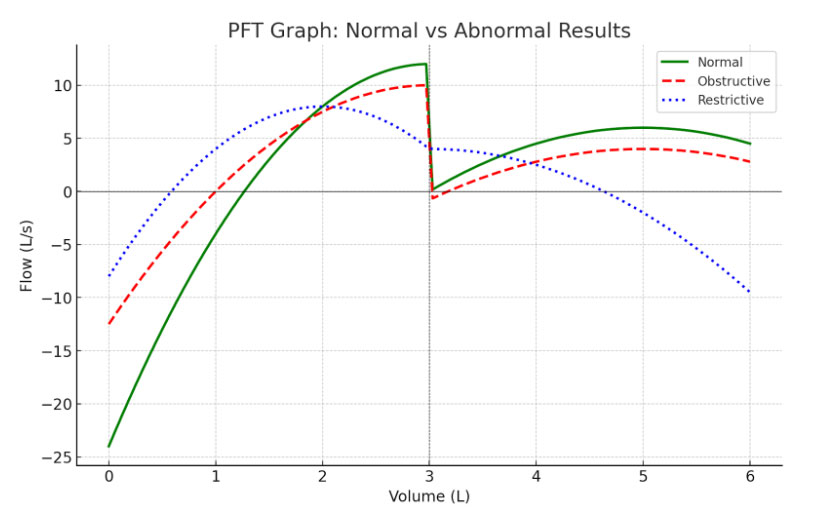
Here is a Pulmonary Function Test (PFT) graph comparing normal and abnormal results:
- Green Line (Normal): Represents a normal flow-volume loop, showing a smooth curve with a peak flow rate and a gradual decline during exhalation.
- Red Line (Obstructive): Represents an obstructive pattern, typically seen in conditions like COPD or asthma. Notice the “scooped-out” appearance of the expiratory limb and a lower peak flow rate.
- Blue Line (Restrictive): Represents a restrictive pattern, often seen in diseases like pulmonary fibrosis. The overall volume is reduced, but the shape of the curve remains relatively normal.
These patterns help healthcare providers diagnose and differentiate between obstructive and restrictive lung diseases based on the shape and characteristics of the flow-volume loop
Disclaimer: The interpretation of abnormal PFT results must be done in conjunction with clinical history, physical examination, imaging studies (like chest X-rays or CT scans), and possibly other tests such as arterial blood gases (ABGs).
If you need more detailed information or examples related to specific conditions or how these results are used in clinical decision-making, feel free to ask!